Yes, the Pandemic Is Ruining Your Body
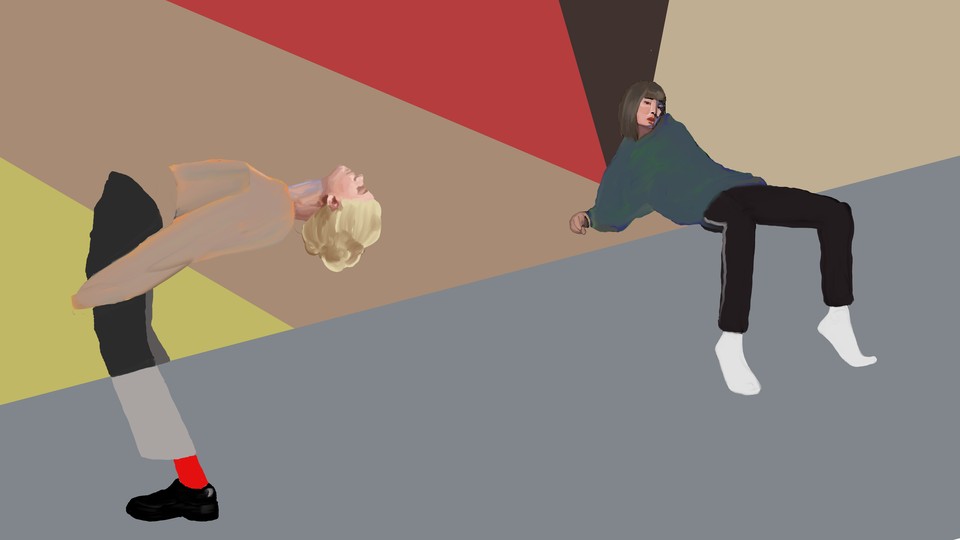
Quarantine is turning you into a stiff, hunched-over, itchy, sore, headachy husk.
The first time my hips locked up, the reason was at least a little bit glamorous. It was 2018, and I was returning from vacation in Sicily, which was the fanciest thing I’d ever done by several orders of magnitude. As I went through the motions—and, perhaps more important, the lack of motion—of international flight, my gait began to stiffen, and my stride contracted to a fraction of its former self. My body, settling into its mid-30s, rebelled against the hours spent in airplane seats, the nights in unfamiliar beds, the constant, awkward physicality of travel.
The same thing happened a few more times over the next year and a half, always after long-haul flights. I began to think of it as “airplane hip,” and the condition was annoying but temporary; I don’t spend much time on planes, and a yoga move called “pigeon pose” would stretch my stiff waddle back into a walk in a day or two. Usually, the discomfort was worth it—a small musculoskeletal price to pay for the occasional privilege of seeing parts of the world still new to me.
One morning in May, I rolled out of bed to find that my hip flexors were at it again. Dragging my rolled-up yoga mat to the middle of the floor to arrange my body into the now-familiar contortion—one leg straight back, the other forward and bent against the floor, then switch—I tried to piece together what was going on. Like most Americans, I hadn’t been on an airplane since February. I had been sitting at home virtually all the time, a situation of relative comfort and incredible luck. But in the weeks that followed, I folded my body into pigeon pose again and again, with minimal returns. As I lost hip flexibility, I also gained other problems, which accumulated over the next several months—low-grade headaches, sore shoulders, a stiff neck, dry skin.
At first, these ailments felt isolated, because my body was isolated. I couldn’t see co-workers also struggling to stretch their back as they got up from their office chair, or friends gobbling up ibuprofen as I was. I couldn’t see anyone doing anything. But as we barrel toward the first anniversary of the World Health Organization declaring the coronavirus a pandemic, the physical consequences of extended disruption, isolation, and stress have begun to make themselves known en masse, in doctors’ offices and telehealth video calls. The coronavirus itself, of course, has had a devastating impact on the physical health of millions of Americans. But even for those who have avoided the virus so far, the by-products of living through an extended disaster have often been painful; for some, they’ve been catastrophic. Even if you don’t get COVID-19, the pandemic might destroy you anyway.
It’s too early for expansive data on how (and how much) people were hurting in 2020, but according to doctors and health-care workers, some clear trends have emerged, and the complaints stretch to the far reaches of the human body. Among the earliest and most enduring have been the type I’ve experienced—aches and pains that emerge without obvious injury, then stick around. “By May, I was seeing a lot more neck and upper back pain, also accompanied with headache,” Jaspal Singh, a pain- and rehabilitation-medicine specialist at Weill Cornell Medicine in New York, told me in an email. These problems have since taken over Singh’s practice—he estimated that before the pandemic, 70 percent of his patients were complaining of lower-back and leg pain. Now more than half have the kinds of aches that come from hours at ad hoc workstations—curving your shoulders forward, jutting your head out in front of your body to look at a laptop whose screen is too low, and maintaining that position for hours at a time, all while sitting in a chair meant to support a human for the duration of a meal, not a workday.
And people aren’t just working in more challenging physical circumstances; they’re also spending more time doing it. “In the office, people work for eight or nine hours, but now they find themselves working 10 or 12 hours at home just because there’s no commute time,” Natalia Ruiz, a physical therapist at NYU Langone Orthopedic Center, told me of her patients. “Expectations of productivity have increased because you’re working from home.” In her practice, she’s seen more complaints of back and neck pain, but also more “repetitive strain” injuries such as carpal tunnel syndrome, tendinitis in the hands and forearms, and pinched nerves in the elbows.
The circumstances of work have changed in some way for millions of Americans, whether that has meant working from home, working longer and more physically punishing hours, or being laid off and largely stuck at home to job-search online. The problems emerging in doctors’ offices are mostly those bothering people who can work from home, because, among other reasons, their jobs are more likely to offer health insurance and time off to seek care than those held by essential workers. People who suddenly shifted to working from home were caught without the basic ergonomic equipment found in many offices, such as adjustable-height desk chairs and laptop stands that can raise screens up to eye level. Some people cobbled together healthier setups as it became clearer how long they would be out of the office, but for many who have lost work or taken pay cuts, spending hundreds of dollars on equipment isn’t feasible. For those living in cramped housing with kids who go to Zoom school and other family members who also need space to work, building a personal mini office simply isn’t an option.
For people who aren’t of working age, the orthopedic concerns are a little different. Elderly people, who are at the highest risk from the virus itself, have also experienced some of the worst physical consequences of isolation. “The elderly are not taking their walks and are getting weaker in their legs,” Singh said. “They are losing confidence in their gait, which causes further weakness, and they enter a vicious cycle.” Many people have sharply reduced their exercise this year as gyms have closed, or they fear catching the coronavirus at those that have reopened, but for younger adults, who are generally more physically fit and less prone to injury, regaining some movement in creative ways is easier, and novel, unsupervised exercise is less risky (although Singh noted that he has seen some injuries from people who have used their new Pelotons vigorously but incorrectly). For older Americans, maintaining a baseline of essential flexibility and stamina while isolated increases the risk of an unsupervised fall—a source of potentially deadly injuries that appears to have become more common since early 2020.
On average, kids are more resilient in the face of the physical stresses of isolation than their brittler-bodied parents or grandparents, but watching online classes—and skipping recess, gym class, and all the incidental opportunities to be rambunctious with friends that in-person school provides—has still taken a toll on many children. Nancy Durban, a pediatric physical therapist at Cincinnati Children’s Hospital, told me that a combination of increased anxiety and uncomfortable computer setups has created a pain spiral for some of her patients. Anxiety “increases their muscle tension, which then makes them hurt more, which makes them move less, which makes them then sleep worse,” Durban told me. “That increases their anxiety and decreases their ability to move again.” As some schools have reopened and resumed extracurricular activities, she has also noted an uptick in sports injuries among kids, who might not have understood that months of isolation diminished their physical capacity to play soccer or run track, or who were simply overexcited to be back with their teammates.
It’s not just our muscles and bones that are burdened. People spending more time gazing at screens have found that their vision is suffering, too. “When people stare at the screen all day, they don't blink very often, and their eyes tend to dry out,” Sunir Garg, an ophthalmologist, clinical spokesperson for the American Academy of Ophthalmology, and professor at Wills Eye Hospital in Philadelphia, told me. “When the eyes feel kind of dry, scratchy, and prickly, it can make things blurry.” That can be exacerbated by spending all your waking hours indoors, in bone-dry heating and cooling systems.

Even for people who spent their workdays indoors and on a computer before the pandemic, the routine of going into work—the process of getting dressed, going outside, getting in a car or boarding a train, interacting with co-workers, attending a meeting or two, and maybe going to happy hour afterward—likely provided enough variation and visual novelty to head off some of the vision problems people are having now. One thing Garg cautions against faulting, though, is the light given off by computers and phones—so-called blue-light glasses have become a hot commodity in the past year; sales of at least one brand have more than doubled as people look for ways to soothe their strained, tired eyes. Absorbing that light in the evenings can throw off sleep patterns, but there is no evidence that it harms vision or strains eyes. “There’s a ton of blue light coming from the sun,” Garg said. “When most people had outdoor jobs, we were getting oodles more blue light from the sun than we ever would from our screens.”
The pandemic also seems to be causing a litany of skin and hair issues, according to research provided by the American Academy of Dermatology, some of which has not yet been published and has yet to be peer-reviewed. The number of reported eczema flares on the hands has increased during the pandemic, a phenomenon thought to be caused by more frequent hand-washing and use of hand sanitizer. Other dermatological problems that have spiked in the past year are closely tied to emotional well-being. Hair shedding is a common symptom of extreme stress, and one study of two hospitals in some of the low-income New York City neighborhoods hit hardest by the pandemic’s first surge found a 400 percent increase in reported hair loss over the summer. Another recent study found that self-reported symptoms of “body-focused repetitive behaviors,” such as skin-picking, nail-biting, and hair-plucking, have increased during the pandemic. When people are suffering inside, those struggles often make their way to the surface.
For many people, the physical ramifications of a year or more in isolation will be temporary, or at least largely reversible. For some, though, the accumulated toll of the pandemic’s disruptions to daily life could be deadly. All the doctors I spoke with worried about patients delaying or avoiding care because of the potential for coronavirus exposure in doctors’ offices or hospitals. Athena Poppas, the president of the American College of Cardiology and the chief of cardiology at Brown University, said that she saw the dire consequences of that fear almost immediately, during the virus’s first surge. “When patients did come in, they were coming in late or very sick, and we had very few options for them,” she told me. People died of heart attacks who might otherwise be alive today.
Poppas worries that isolation’s worst cardiovascular ramifications may be ahead of us, though. Depression and anxiety, both of which have surged among Americans during the pandemic, are enormous risk factors for heart problems, especially among people over 50. Quarantine itself is also a risk factor. “Loneliness and social isolation increase the risk of myocardial infarction and stroke by up to 30 percent,” she told me. “I had a patient who said she hasn’t seen [anybody else] in months, and it just broke my heart.”
The early symptoms of these problems can be subtle, and in isolation, they may go unnoticed. “It might have been their neighbor who saw them every day who said, ‘Gee, Mr. Jones, you seem more short of breath,’” Poppas told me. “In addition to the internal problem, there’s not the external social checks.” She has noticed that some of her patients, without the support and interaction they’d usually have from family, home health aides, or even chance encounters with acquaintances, have been less likely to take their medication on schedule, keep up with at-home health routines, stay hydrated, or eat a balanced diet.
While Poppas described these problems, I thought of how most of them had shown up, in lesser ways, in my own life. In the past year, I’ve lost 30 pounds from terror and then gained it back from stress eating. At some point in the past few months, I switched from three meals a day to two, because the third simply did not feel worth the effort. As I type this, my head is pounding for reasons that are not clear to me. If I had to guess, I’d say it is related to how I am sitting in my chair, where I’ve been for hours. I try to keep my water bottle filled, but right now, I don’t know where it is in my apartment. And I’m one of the lucky ones.
The consequences of the past year for our bodies are, as far as I can tell, limitless. In the richest nation in the world, an obscene—and rising—number of people cannot afford to feed themselves. People are cracking their teeth from mental and physical stress. Millions of people now spend little time in shoes, which is screwing up their feet.
It didn’t have to be like this. Those in power in the United States could have decided to take the pandemic seriously, and after a few months we could have returned to more normal versions of our lives, as people across the globe have done. Instead, we’ve been strapped into an interminable long-haul flight for months, with all of the stress and expense and discomfort that the worst of air travel implies—except we’ve gone nowhere.